At first glance, OCPD and OCD look almost identical—the similar names alone cause a ton of confusion for parents. But the truth is, they are fundamentally different conditions, and that difference hinges on a single, crucial question: How does your child feel about their own thoughts and behaviors?
The answer is the key to telling them apart. OCD is driven by unwanted, intrusive thoughts (ego-dystonic) that cause intense anxiety, while OCPD is a personality style where the child sees their rigid rules and perfectionism as correct and beneficial (ego-syntonic). Your child's own self-awareness, or lack thereof, is the biggest clue you have.
Decoding OCD and OCPD for Parents
When you're trying to figure out what's going on with your child, understanding the core distinction between these two is the first step toward getting them the right kind of help. An integrative approach that considers therapy, nutrition, and healthy habits offers the most comprehensive support.
Obsessive-Compulsive Disorder (OCD) is an anxiety disorder. It traps a child in a painful cycle of distressing, unwanted obsessions and the compulsive behaviors they perform to try and quiet the anxiety. They know the thoughts are irrational, and they hate it.
In contrast, Obsessive-Compulsive Personality Disorder (OCPD) is a personality disorder, defined by a deep-seated, all-encompassing need for perfectionism, order, and control. A child with OCPD genuinely believes their way of doing things is the right way—and they often expect everyone else to follow their lead.
This perception gap—whether the behaviors are a problem to be solved or a strength to be proud of—shapes everything from your child's relationships to their willingness to even consider that they need help.
While they sound similar, OCPD is actually much more common. It affects an estimated 2-7% of people, whereas OCD affects about 1.2% of the U.S. population. Despite being more prevalent, OCPD often flies under the radar because its traits can easily be mistaken for a "strong work ethic" or just having "high standards." You can read the full research about these OCPD statistics to see how this impacts diagnosis.
This infographic breaks down the core emotional drivers in a really simple way.
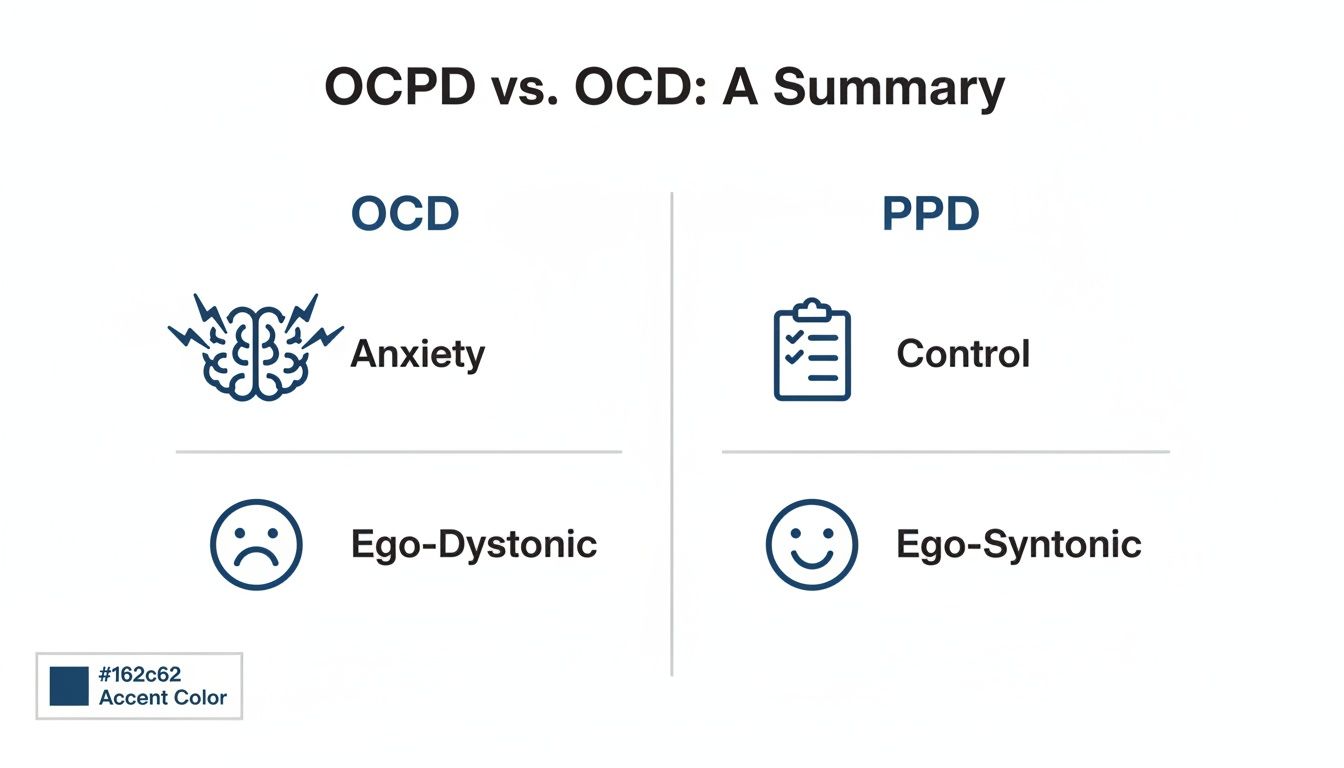
As the image shows, a child with OCD is suffering internally from anxiety. A child with OCPD, on the other hand, is driven by a need for control and a firm belief that their way is the best way.
OCPD vs OCD Key Distinctions at a Glance
For parents trying to make sense of their child's behaviors, sometimes a quick side-by-side comparison is the most helpful tool. This table zeroes in on the practical differences you're likely to see at home.
| Characteristic | Obsessive-Compulsive Disorder (OCD) | Obsessive-Compulsive Personality Disorder (OCPD) |
|---|---|---|
| Core Motivation | To stop the anxiety caused by unwanted, intrusive thoughts. | To achieve perfect order, flawless results, and complete control. |
| Child's Insight | Ego-dystonic: The child is deeply distressed by their obsessions and compulsions and knows they don't make sense. | Ego-syntonic: The child sees their rigid behaviors and rules as logical, correct, and even superior. |
| Focus of Behaviors | Specific, ritualistic compulsions tied to specific fears (e.g., hand washing to prevent sickness). | Pervasive perfectionism and control that applies to almost everything (school, chores, hobbies, friendships). |
| Impact on Others | The child’s internal distress is the primary problem. | The child's rigidity and demands for control often create major conflict with family, friends, and teachers. |
Think of it this way: A child with OCD is a prisoner to their thoughts. A child with OCPD sees themselves as the warden, enforcing what they believe are necessary rules for a better, more orderly world. Recognizing which role your child has fallen into is the first step toward helping them find relief.
Comparing Symptoms in Children and Teens
The best way to grasp the difference between OCPD and OCD is to see how they show up in a child's day-to-day life. While both can look like rigid, repetitive behavior on the surface, what’s going on inside a child’s head is completely different. For a child with OCD, their actions are a frantic attempt to shut down overwhelming anxiety. But for a child with OCPD, those same behaviors are about achieving a level of perfection they genuinely believe is the right way to do things.

Let's take a real-world example. Imagine a child who is terrified of germs. If they have OCD, this obsession might compel them to wash their hands until their skin is raw and cracked. The goal isn't just about being clean; it's a specific, ritualistic act they have to perform to silence the intrusive thought that they're contaminated. They feel driven to do it, even if a part of them knows it’s excessive.
Now, picture a teen with OCPD. They might spend hours organizing their school binder, making sure every paper is perfectly aligned by subject, date, and even font size. This isn't fueled by a specific fear. It's driven by an unwavering belief that this is the only correct way to organize a binder. They might miss homework deadlines because the binder isn't "done" yet, but in their mind, their meticulous system is a strength, not a problem.
The Internal Experience: Ego-Dystonic vs. Ego-Syntonic
A child with OCD is in a constant state of distress. They’re fighting against thoughts they know are irrational, intrusive, and not their own. This internal battle is known as being ego-dystonic—their obsessions and compulsions feel foreign and are in conflict with their true self.
On the other hand, a child with OCPD sees their traits as ego-syntonic. Their rigid rules, perfectionism, and need for order feel completely natural and correct to them. They don't view their sky-high standards as a problem. In fact, they often get frustrated when others don't share their commitment to doing things the "right" way. Grasping this core difference is crucial for parents. For a deeper dive, check out our guide on the signs and symptoms of pediatric OCD.
It's also worth noting that gender can play a role in diagnosis. OCPD is diagnosed about twice as often in males as in females. OCD, however, shows the opposite pattern, with a higher prevalence in women than in men.
Creating a Supportive Environment at Home
Alongside professional treatment, parents can create a home environment that promotes better brain function and emotional regulation. This holistic approach focuses on simple lifestyle factors that have a big impact.
- Brain-Healthy Nutrition: Focus on affordable, nutrient-dense foods. Deficiencies in key minerals and vitamins, like magnesium, zinc, and B vitamins, can affect mood. Simple additions like beans, lentils, nuts, and leafy greens are a great, budget-friendly start.
- Omega-3 Supplementation: Omega-3 fatty acids, especially EPA and DHA found in fish oil, are vital for brain health and can help reduce inflammation. Look for a high-quality supplement with a good concentration of EPA and DHA. For plant-based families, algae-based options are a fantastic alternative.
- Daily Movement: Never underestimate the power of exercise. Family walks, bike rides, or just a silly dance party in the living room can boost mood-regulating neurotransmitters like serotonin and dopamine, which helps improve cognitive flexibility and melt away stress.
- Structured Routines: A predictable schedule is calming for an anxious brain. Consistent times for waking up, eating meals, and going to bed help regulate the body's natural rhythms, providing a stable foundation for a child's emotional state.
Important Disclosure: The information provided here is for educational purposes only and is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of a qualified healthcare professional with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read here, especially when considering medications or supplements for your child.
Navigating Diagnostic Challenges and Comorbidity
Telling the difference between OCPD and OCD in a child can be tricky, especially since the two conditions can show up together. This overlap is known as comorbidity, which simply means a child can have both OCPD and OCD at the same time. Naturally, this complicates things, making an accurate diagnosis and an effective treatment plan that much harder to pin down. A comprehensive psychiatric evaluation is the only way to really untangle these overlapping symptoms.

The main tool professionals use to separate the two is figuring out if the behaviors are ego-syntonic (OCPD) or ego-dystonic (OCD). A child with OCPD genuinely sees their rigid rules and routines as correct and valuable. On the other hand, a child with OCD is deeply distressed by their unwanted thoughts and compulsions. This internal experience is the most important clue for a clinician.
Understanding Co-Occurring Conditions
It's very common for both OCPD and OCD to appear alongside other mental health conditions, which can muddy the diagnostic waters even more. Knowing about these common pairings helps parents and professionals build a more complete and supportive treatment strategy.
For a child with OCPD, their constant perfectionism and rigidity often spill over into other challenges. Common comorbidities include:
- Anxiety Disorders: The relentless pressure to be perfect can easily fuel persistent worry and anxiety.
- Depression: When a child constantly falls short of their own impossible standards, it can lead to feelings of failure and hopelessness.
- Eating Disorders: The intense need for control can manifest in rigid, unhealthy eating habits.
Similarly, the distress that comes with OCD often travels with other conditions. For OCD, common co-occurring disorders are:
- Other Anxiety Disorders: Social anxiety and panic disorder are frequent companions to OCD.
- Tic Disorders: There's a well-established link between OCD and conditions like Tourette's syndrome.
- ADHD: The executive function challenges in ADHD can overlap with and worsen OCD symptoms. You can learn more about how ADHD increases the risk for co-morbid conditions in our detailed guide.
Research really drives home how significant this overlap is. Among people diagnosed with OCD, a striking 58.8% also meet the criteria for comorbid OCPD. What's more, OCPD is frequently linked with mood disorders (in 24% of cases) and other anxiety disorders (in 23-24% of individuals), which makes both diagnosis and treatment a complex puzzle.
The Role of Psychotropic Medications
When a child is diagnosed with OCPD, OCD, or a combination of both, medication can be an important piece of a balanced treatment plan. These medications aren't a cure, but they can support healthier brain function, which in turn makes therapy much more effective.
Medications like Selective Serotonin Reuptake Inhibitors (SSRIs) help regulate neurotransmitters like serotonin, a key player in mood and anxiety. For a child struggling with OCD, this can feel like turning down the volume on those intrusive thoughts, giving them the mental breathing room to engage in therapy. For a child with OCPD, medication might help ease some of the rigidity and improve their ability to regulate emotions.
By helping to stabilize brain chemistry, these medications can unlock a child's potential to learn new coping skills and build resilience. It is absolutely crucial to consult with a qualified child psychiatrist to determine if medication is a safe and appropriate option for your child.
Disclaimer: This information is for educational purposes only and is not intended to diagnose or treat any medical condition. Always consult with a qualified healthcare professional to discuss your child's specific needs, especially when considering medications or supplements.
Putting Together a Treatment Plan for Your Child
When you're trying to figure out the difference between OCPD and OCD, it's important to know that the right treatment plan has to support your child's whole well-being. A solid approach usually weaves together targeted therapy with smart strategies that boost brain health from different angles—think nutrition, daily habits, and sometimes, medication. The aim is to build a strong foundation so your child can develop resilience and learn healthier ways of thinking and acting.
For OCD, the undisputed champion of treatments is a specific form of Cognitive Behavioral Therapy (CBT) known as Exposure and Response Prevention (ERP). This therapy guides children to gradually face their fears (the exposure part) without giving in to the compulsive rituals they use to feel better (the response prevention part). With time and practice, this process essentially rewires the brain to see that the scary outcomes don't actually happen, which takes away the power of the obsessions.
OCPD, on the other hand, often needs a different kind of therapeutic approach. Since kids with OCPD genuinely believe their way of doing things is the right way, therapies like psychodynamic therapy or a modified version of CBT tend to work better. These methods help the child gain insight into how their rigid perfectionism is affecting their relationships and happiness, gently nudging them toward more flexibility.
The Role of Medication in Brain Health
Sometimes, therapy alone isn't enough to get the ball rolling, and that's when medication can be a really helpful partner in the process. It’s crucial for parents to see these medications not as a "cure," but as a tool to help rebalance brain chemistry. This can make the hard work of therapy feel more manageable and effective for a child who is struggling.
Selective Serotonin Reuptake Inhibitors (SSRIs) are a class of medication frequently prescribed for both OCD and OCPD. They work by boosting the levels of serotonin—a key chemical messenger in the brain that helps regulate mood, anxiety, and impulse control.
- For a child with OCD, an SSRI can dramatically lower the volume on those loud, distressing, and intrusive thoughts. This creates some much-needed mental breathing room, making it possible for them to really dig into ERP therapy without feeling completely overwhelmed by anxiety.
- For a child with OCPD, while the research isn't as direct, SSRIs can help ease the underlying anxiety and inflexibility that often drive their perfectionistic behaviors. By helping them better regulate their emotions, the medication can make them more open to the idea of trying new, more flexible ways of behaving.
These medications support healthier brain function, which unlocks your child’s ability to learn and use new coping skills. A conversation with a child psychiatrist is the essential next step to figure out if medication is a safe and appropriate choice for your child.
Supporting Treatment with Diet and Healthy Habits
A truly comprehensive plan goes way beyond the therapist's office. Simple, consistent daily routines can make a huge difference in your child’s mental health by giving their brain what it needs to function at its best.
Think of food as fuel for the brain. When key nutrients are missing, especially minerals like magnesium and zinc or various B vitamins, it can directly impact mood and thinking. Sticking to an affordable, whole-foods diet filled with fruits, vegetables, lean proteins, and whole grains gives the brain the building blocks it needs to thrive. Cutting back on processed foods and sugary snacks, which can fuel inflammation and mood swings, is another powerful move. You can explore more ideas in our guide with 14 effective ways to help your child overcome OCD at home.
The Power of Supplements and Exercise
Certain supplements can also offer extra support. Omega-3 fatty acids, especially the EPA and DHA found in fish oil, are vital for brain health and have been shown to help reduce inflammation. When picking a supplement, look for a trustworthy brand with a high concentration of EPA and DHA. For a more budget-friendly approach, try adding omega-3-rich foods like salmon, flaxseeds, or chia seeds to your meals. Algae-based supplements are a great option for plant-based families.
Finally, don't underestimate exercise. It’s one of the most potent brain-healthy activities there is. Physical activity naturally boosts mood-lifting brain chemicals like serotonin and dopamine. It also sharpens cognitive flexibility—the brain’s ability to shift between different thoughts or tasks, which is a major hurdle for kids dealing with OCPD or OCD.
Disclaimer: This information is for educational purposes only and is not intended to diagnose or treat any medical condition. Always consult with a qualified healthcare professional to discuss your child's specific needs, especially when considering medications or supplements.
Supporting Brain Health Through Nutrition and Diet
When we take an integrative approach to managing OCPD or OCD in children, we always have to talk about nutrition. The food a child eats literally provides the building blocks for brain health, directly impacting everything from neurotransmitter function and mood regulation to cognitive flexibility. By focusing on a nutrient-dense diet, you create a powerful biological foundation that makes formal treatments even more effective.
Many parents I’ve worked with find that making small, consistent dietary changes can have a surprisingly noticeable impact. This isn’t about chasing perfection; it’s about making progress and giving your child's brain the fuel it needs to function at its best.
The Impact of Diet and Unhealthy Habits
It's no secret that diets high in processed foods, sugar, and unhealthy fats can contribute to inflammation and mood instability. For a child struggling with rigidity or anxiety, this can make symptoms even worse. These foods can throw off the delicate balance of gut bacteria—which we now know is deeply connected to mental health—and cause energy spikes and crashes that make it harder for a child to regulate their emotions.
Simple swaps can make a huge difference. For example, replacing a sugary breakfast cereal with a bowl of oatmeal and berries provides sustained energy and fiber, which helps support a healthy gut microbiome and a more stable mood throughout the morning.
Key Nutrients for Brain Function
Sometimes, specific nutritional deficiencies are linked to challenges with mental wellness. Making sure your child gets enough of these key vitamins and minerals can be a simple, affordable way to support their brain.
- Magnesium: Often called the "calming mineral," magnesium plays a vital role in regulating the nervous system. You don't need expensive supplements to get it—affordable sources include beans, lentils, nuts, seeds, and leafy greens.
- Zinc: This mineral is crucial for neurotransmitter function. It's found in lean meats, legumes, and even pumpkin seeds.
- B Vitamins: Essential for producing energy and creating mood-regulating brain chemicals, B vitamins are abundant in whole grains, eggs, and dark leafy vegetables.
Remember, a balanced diet filled with whole foods is the best way to ensure your child gets these vital nutrients. Focusing on affordable options like legumes, seasonal vegetables, and whole grains makes healthy eating achievable for any family.
The Role of Omega-3 Supplements
Omega-3 fatty acids, especially EPA (eicosapentaenoic acid) and DHA (docosahexaenoic acid), are superstars for brain health. They are critical parts of brain cell membranes and have powerful anti-inflammatory properties, which can help support neurotransmitter function and reduce anxiety.
When you’re looking for an Omega-3 supplement for your child, quality and the right formulation are what matter most.
- Check EPA/DHA Levels: Look for a supplement that clearly states the amount of EPA and DHA per serving. A higher concentration is usually better.
- Choose the Right Type: Fish oil is the most common source, but for families on a plant-based diet, algae-based supplements offer a high-quality, vegan source of both EPA and DHA.
- Ensure Purity: Stick with reputable brands that test their products for heavy metals and other contaminants. This ensures both safety and purity.
Incorporating these nutritional strategies can help make your child's brain more resilient and more receptive to the hard work they’re doing in therapy.
Disclaimer: This information is for educational purposes only and is not intended to diagnose or treat any medical condition. Please consult with a qualified healthcare professional before starting any new diet or supplement regimen for your child.
Weaving Brain-Healthy Habits Into Daily Life
Formal treatments for OCPD or OCD are crucial, but what you do at home day-to-day can make a huge difference. Think of it as creating a supportive environment where your child’s brain can thrive. By building consistent, brain-healthy habits, you help your child develop resilience, handle their emotions better, and just feel more grounded.
These small, daily actions create a stable foundation that actually makes therapy and medication work better. It’s not about being perfect; it’s about consistent effort. Erratic sleep schedules, a couch-potato lifestyle—these things can mess with brain chemistry and make symptoms like anxiety and rigidity worse. Predictable routines and positive choices, on the other hand, create a sense of safety and control that is incredibly calming for a child's nervous system.
The Power of Exercise
If you do just one thing, get them moving. Exercise is one of the most powerful brain-healthy activities a child can do. It’s not just about burning off steam; physical movement is a natural way to boost mood-regulating neurotransmitters like serotonin and dopamine. These are the exact brain chemicals that create feelings of well-being and can even improve cognitive flexibility—a real challenge for kids with OCPD or OCD.
The key is making it fun and easy, so it sticks. You don't need a gym membership or fancy gear.
- Family Bike Rides: A simple cruise around the block gets everyone moving and doubles as quality time together.
- Dance Parties: Throw on their favorite playlist and have a five-minute dance-off in the living room.
- Team Sports: If your child likes being around other kids, team sports are a great way to build physical fitness and social skills at the same time.
- Nature Walks: Just spending time outdoors has been proven to lower stress and sharpen focus.
Creating a Supportive Daily Routine
Beyond getting their heart rate up, other daily habits play a huge role in mental wellness. A truly integrative approach sees that sleep, relaxation, and creativity are just as vital as what they eat or how much they run around.
A consistent sleep schedule is absolutely non-negotiable for brain health. Try to stick to the same bedtime and wake-up time every day, even on weekends, to keep your child’s internal clock regulated. Simple mindfulness tricks can also be surprisingly effective. For instance, teaching them "box breathing"—inhale for four counts, hold for four, exhale for four, hold for four—for just a minute can quiet an anxious mind right down.
Don’t underestimate creative hobbies. Things like drawing, playing an instrument, or building with LEGOs provide a healthy way to channel stress. It also lets a child feel a sense of accomplishment that isn't tied to rigid, rule-based tasks.
A Sample Brain-Healthy Daily Flow
So, what does this look like in real life? Here’s a simple way to fit these pieces into a typical day to boost mental wellness:
- Morning (7:00 AM): Kick things off with a solid breakfast. Think oatmeal with berries and a sprinkle of nuts to provide sustained energy and brain-loving omega-3s.
- After School (3:30 PM): Carve out 30 minutes for active play—ride bikes, kick a soccer ball around, or just walk to the park.
- Downtime (5:00 PM): Encourage a screen-free, creative activity. This is a great time for drawing or just listening to music to decompress from the day.
- Evening (8:00 PM): Start a calming wind-down routine. A few minutes of quiet reading or some deep breathing exercises before a consistent bedtime works wonders.
These aren't massive, life-altering changes. They're small, consistent actions that send a powerful signal to your child’s brain, reinforcing patterns of calm, stability, and resilience that will powerfully support them on their journey.
Your Questions Answered
When you're trying to understand the differences between OCPD and OCD, it’s completely normal to have a lot of questions. Here are some clear, straightforward answers to the concerns I hear most often from parents, designed to help you support your child and make informed decisions.

Can My Child Outgrow OCD Or OCPD Without Treatment?
While the intensity of symptoms can certainly ebb and flow, both OCD and OCPD are considered chronic conditions. They don't typically just go away on their own and usually require professional treatment to manage effectively.
Starting early with proven therapies gives your child the best long-term outlook. An integrative plan that weaves together therapy, good nutrition, and healthy routines builds coping skills that will serve them for a lifetime. For instance, something as simple as daily exercise can help regulate mood-stabilizing neurotransmitters, making the work they do in therapy even more powerful.
How Do I Talk To My Child About Their Behaviors?
The most important thing is to approach the conversation from a place of love and curiosity, not judgment. Try using "I" statements to share what you've observed. For example, you could say, "I've noticed you seem to need things to be just right, and it looks like that's making you feel really stressed."
This shifts the focus to the emotion behind the action (like anxiety or frustration) instead of criticizing the behavior itself. It opens the door for a real conversation.
The goal is to validate their feelings while gently suggesting there are ways to make things feel less overwhelming. This creates a safe, supportive space for them to even consider getting help.
Is There A Single Test To Diagnose The Difference?
No, there isn't one single blood test or brain scan that can distinguish between OCPD and OCD. A diagnosis comes from a skilled mental health professional through a very thorough process.
This involves in-depth clinical interviews, observing behaviors, and sometimes using standardized assessment tools. It's a detailed evaluation designed to get a true picture of your child's internal world and how it shows up in their actions.
What Role Do Psychotropic Medications Play?
Medications, especially SSRIs (Selective Serotonin Reuptake Inhibitors), can be an incredibly helpful piece of the puzzle. They work by helping to regulate brain chemicals like serotonin, which can improve mood and dial down anxiety.
For a child with OCD, this might mean quieting the storm of intrusive thoughts, which makes therapy much more effective. For a child with OCPD, it might soften some of the rigidity. These medications don’t fix the problem on their own, but they can support brain function, making it easier for your child to engage with and benefit from therapy. It's crucial to consult a child psychiatrist to determine if medication is the right choice.
Disclaimer: This information is for educational purposes and is not intended to diagnose or treat any medical condition. Always consult with a qualified healthcare professional when discussing medications or supplements for your child.
At Children Psych, we believe in a comprehensive approach to child mental wellness, combining evidence-based treatments with practical support for families. If you're concerned about your child's mental health, we're here to help. Learn more and schedule a consultation at https://childrenpsych.com.