Let's get one of the most common questions out of the way first: What's the real difference between ADD and ADHD?
The short answer is simple: ADD is an outdated term. What many of us grew up calling Attention Deficit Disorder (ADD) is now officially known as Attention Deficit Hyperactivity Disorder (ADHD), Predominantly Inattentive Presentation. This isn't just a name change; it reflects a much deeper understanding that hyperactivity isn't a mandatory ingredient for an ADHD diagnosis.
Understanding the Shift from ADD to ADHD
If you find the ADD vs. ADHD terminology confusing, you're not alone. The terms are still used interchangeably in everyday conversation, but in a clinical setting, the language is very specific and has a history behind it. The term ‘ADD’ was officially retired decades ago to better paint a picture of the condition's full spectrum.
The big change happened back in 1994 when the American Psychiatric Association published the DSM-IV. They dropped ‘ADD’ and replaced with ‘ADHD,’ which stands for Attention Deficit Hyperactivity Disorder. Why? This update acknowledged that the condition often includes challenges with hyperactivity and impulsivity, not just trouble paying attention. You can actually read some of the historical research behind these diagnostic changes to see how our understanding has evolved.
This evolution brought us to the three official "presentations" of ADHD we use today:
- Predominantly Inattentive Presentation: This is what used to be called ADD. It’s marked by challenges with staying focused, getting organized, and actually finishing tasks.
- Predominantly Hyperactive-Impulsive Presentation: This type looks more like what people traditionally picture as ADHD. It involves restlessness, blurting things out, interrupting others, and acting on impulse.
- Combined Presentation: This is the most common diagnosis. It means a person shows significant symptoms of both inattention and hyperactivity-impulsivity.
Realizing this isn't about two separate disorders is a key first step. It’s about one condition that can show up in different ways.
Comparing Old and New ADHD Terminology
To make this crystal clear, here’s a quick reference table. It’s designed to help you connect the old term you might hear on the playground with the correct clinical language a professional will use.
| Outdated Term | Current ADHD Presentation (DSM-5) | Key Characteristics |
|---|---|---|
| Attention Deficit Disorder (ADD) | ADHD, Predominantly Inattentive Presentation | Difficulty sustaining attention, forgetfulness, easily distracted |
| Attention Deficit Hyperactivity Disorder (ADHD) | ADHD, Predominantly Hyperactive-Impulsive or Combined Presentation | Restlessness, impulsivity, constant movement, and/or a mix of inattentive symptoms |
So, when you hear someone mention ADD, they're likely describing the inattentive presentation of ADHD. Knowing the modern terms will help you have more productive conversations with doctors, teachers, and therapists, ensuring everyone is on the same page about your child's specific challenges.
Recognizing How ADHD Symptoms Appear in Real Life
Knowing the clinical definitions is one thing, but seeing how ADHD symptoms actually play out day-to-day is what really brings it all into focus. The difference between the various presentations often boils down to distinct patterns of behavior you might see at home or get reports about from school. These patterns help parents tell the difference between what used to be called ADD and the more hyperactive forms of ADHD.
The infographic below really helps visualize how the old term "ADD" has evolved into the broader ADHD diagnosis we use today, showing how it now functions as an umbrella term.
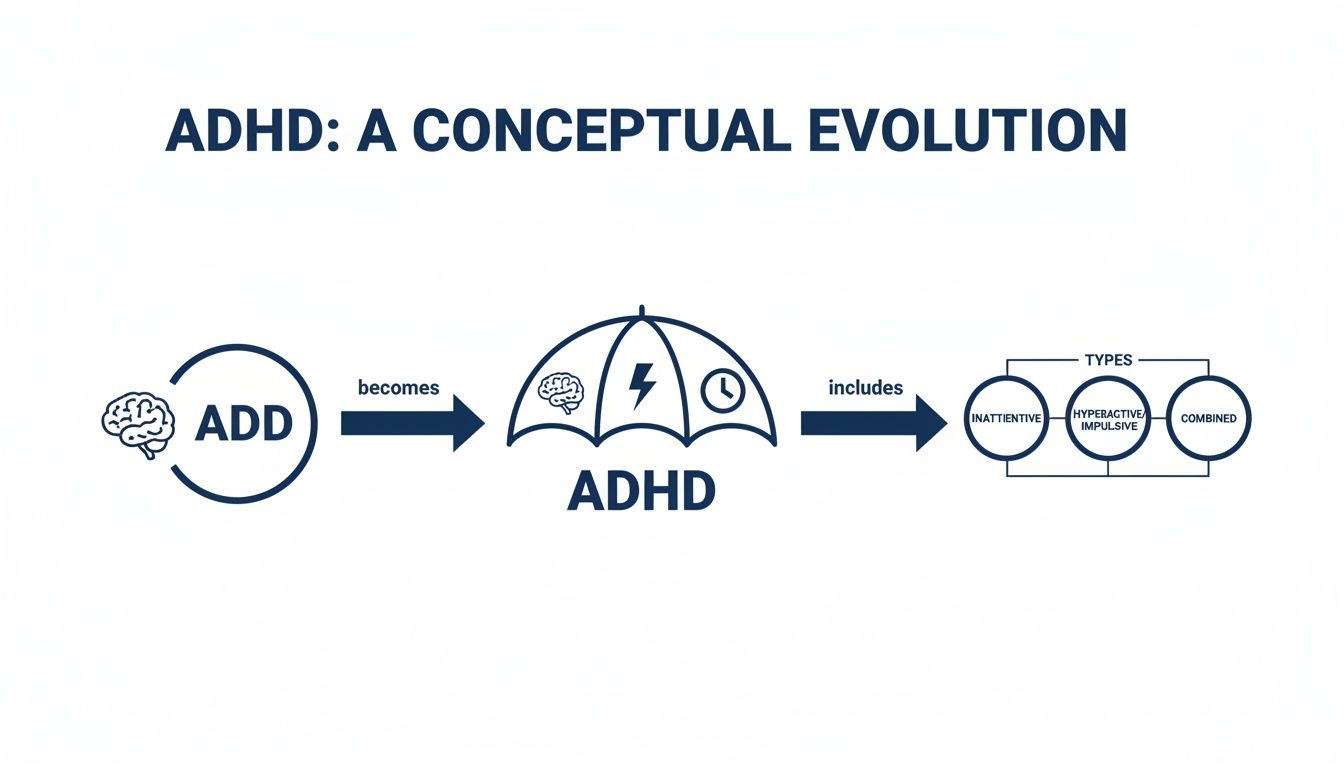
As you can see, "ADD" isn't a separate diagnosis anymore. It’s simply one specific presentation—the inattentive type—that falls under the main ADHD diagnosis, alongside the hyperactive and combined types.
The Inattentive Presentation: The Daydreamer
A child with the Predominantly Inattentive Presentation might be the one you'd call a "daydreamer" or describe as "spacey." This is the classic profile of what was once known as ADD. In real life, this is the child who has a tough time with any task that requires sustained mental effort.
For instance, you might ask them to clean their room, only to find them 20 minutes later completely sidetracked after putting away a single toy. They constantly misplace their jacket, homework, or lunchbox, and often seem like they aren’t listening even when you're speaking directly to them. It’s less about defiance and more about a genuine struggle with organization and focus.
At its core, the inattentive presentation is a challenge of executive function. It’s not a lack of intelligence or willingness, but a struggle to initiate, organize, and follow through on multi-step instructions.
The Hyperactive-Impulsive Presentation: The Mover
On the flip side, a child with the Predominantly Hyperactive-Impulsive Presentation seems to have a motor that never stops running. They are always "on the go"—fidgeting, squirming in their chair, or climbing on the furniture when they shouldn't be. Waiting for their turn in a game or standing in line can feel almost physically impossible for them.
In the classroom, this is the student who might blurt out an answer without being called on or frequently interrupt other kids' conversations. Their impulsivity isn't malicious; it comes from an inability to hit the pause button and think before they act.
The Combined Presentation: The Blend
Many kids show a strong mix of symptoms from both categories, which leads to a diagnosis of Combined Presentation. This child might struggle to finish their math homework because they get distracted (inattention) while also constantly tapping their foot and interrupting their siblings (hyperactivity-impulsivity).
This blend can sometimes be the most obvious to spot because it impacts both quiet, focused settings and more active, social ones. The prevalence of these different types varies, but an analysis found the inattentive type is the most common. For a closer look at these behaviors, you can also check out our guide on understanding ADHD symptoms and medications.
The Road to an ADHD Diagnosis
Figuring out if your child has ADHD can feel like a huge, complicated journey. But understanding how a real diagnosis works can bring a lot of clarity and, honestly, a sense of relief. It’s so much more than just ticking off boxes on a checklist. A good evaluation is a deep dive into your child's world—their strengths, their struggles, and what makes them unique. This isn't about slapping on a label; it’s about creating a personalized roadmap that actually helps.
A proper evaluation is also crucial for ruling out other things that can look a lot like ADHD. Sometimes, what seems like inattention is actually anxiety, a hidden learning disability, or even certain nutritional issues. A comprehensive assessment is the only way to be sure your child gets the right support to truly thrive.
We’ve seen a huge jump in ADHD awareness over the years. Back in 2000, only about 6-10% of kids in the U.S. had a diagnosis. By 2022, the CDC reported that number had climbed to 7 million children aged 3-17 (11.4%). With the rise of telehealth, getting a good, evidence-based evaluation is more important than ever.
What a Real Evaluation Looks Like
A thorough diagnostic process pulls together information from several different places, with each piece giving us another part of the puzzle. This multi-angled approach is what leads to an accurate and truly useful diagnosis.
A skilled clinician will want to hear from everyone involved:
- Parent and Child Interviews: This is where we talk—really talk. We’ll go through your child's developmental history, what behavior looks like at home, and how they get along with friends and family.
- School Feedback: Teachers see a side of your child we don't. Their insights on classroom behavior, academic struggles, and social dynamics—often gathered through standardized rating scales—are invaluable.
- Clinical Observation: The psychologist will spend time interacting with and observing your child directly, looking for those specific behavioral markers of inattention, hyperactivity, or impulsivity in real-time.
- Specialized Testing: This can involve specific assessments that measure cognitive skills like attention, memory, and executive function. It helps us pinpoint exactly where the difficulties are.
This kind of rigorous, evidence-based process goes way beyond the simple question of "ADD vs. ADHD." The goal is to understand how your child’s brain is wired, which creates the foundation for support that actually works.
When we take this kind of detailed approach, we can build a plan that is truly customized to your child. For parents just starting down this path, understanding how to navigate an ADHD diagnosis online can shed more light on what to expect from modern evaluations. The best first step is always to consult with a qualified professional.
An Integrative Framework for Managing ADHD
Truly effective ADHD management isn’t about finding a single "magic bullet." Instead, it's about building a supportive, multi-faceted plan that addresses the whole child. Think of it as creating a strong foundation—an integrative framework that combines medical support with powerful, everyday lifestyle strategies to create the most robust system for success.
This holistic approach recognizes that every part of a child's life—from what they eat and how much they sleep to their daily physical activity—has a direct impact on their brain health and overall well-being.

This plan is a partnership between you, your child, and your healthcare provider. The goal is simple: improve focus and reduce challenging symptoms by nurturing the brain from every possible angle.
The Role of Psychotropic Medications
For many families, psychotropic medication is a cornerstone of an effective ADHD plan. It's important to understand that these medications aren't a "cure." They are sophisticated tools designed to improve core brain functions related to attention, impulse control, and executive function. They work by helping key brain chemicals, or neurotransmitters, communicate more effectively, unlocking a child's potential.
There are two primary groups of medications prescribed for ADHD:
- Stimulants: This is the most common and often the first-line treatment. They work by increasing the levels of dopamine and norepinephrine in the brain, which are crucial for attention and focus. For many children, stimulants can bring about a significant improvement in their ability to stay on task, manage impulses, and organize their thoughts.
- Non-Stimulants: These medications work differently, often by targeting norepinephrine. They can be an excellent alternative for children who don't respond well to stimulants or experience bothersome side effects. Non-stimulants can also be helpful for managing emotional regulation and hyperactivity.
Working closely with a qualified child psychiatrist or pediatrician is essential. They are the experts who can determine if medication is appropriate and, if so, which type and dosage will offer the greatest benefit to improve your child's brain function.
Fueling the Brain with Smart Nutrition
You've heard it a million times: "you are what you eat." For a child with ADHD, this couldn't be more true. What a child eats directly impacts their brain function, mood, and focus. A diet centered on brain-healthy foods can be a powerful ally in managing symptoms, while unhealthy habits like consuming excessive processed sugars and artificial additives can sometimes worsen challenges.
Focusing on an affordable, balanced diet rich in whole foods is a fantastic and easily implemented strategy. Simple, impactful changes include:
- Prioritizing Protein: Foods like eggs, lean meats, beans, and nuts are fantastic for maintaining stable blood sugar and improving concentration. An affordable breakfast of scrambled eggs and whole-wheat toast provides lasting energy.
- Incorporating Complex Carbs: Think whole grains, fruits, and vegetables. These provide a slow, steady supply of energy, avoiding the sharp spikes and crashes that come with sugary, processed snacks.
- Addressing Nutritional Deficiencies: Research suggests some children with ADHD may have lower levels of key nutrients like iron, zinc, and magnesium. Your child's doctor can help identify any potential gaps.
An affordable approach is to build meals around whole foods that are in season. For example, a simple breakfast of scrambled eggs (protein) with a side of whole-wheat toast and an apple (complex carbs) can set the stage for a more focused day.
Brain-Healthy Activities and Supplements
Beyond diet, daily habits and certain supplements can provide an extra layer of support. Exercise is hands-down one of the most effective non-medical interventions for ADHD. Physical activity is a powerful brain-booster—it naturally increases dopamine and norepinephrine, improving focus and mood.
Try to aim for at least 30-60 minutes of fun, engaging movement every day. This doesn't have to be a structured sport; bike riding, dancing, or even just a game of tag works wonders.
Supplements can also play a role, especially Omega-3 fatty acids. Found in fish oil, these healthy fats are vital for brain cell structure and communication. When shopping for a supplement, look for one with a higher ratio of EPA to DHA and make sure it is third-party tested for purity. You can often find affordable, high-quality options from reputable store brands. Always consult your healthcare professional before starting any supplement.
An integrative plan brings together the best of all these worlds—medication (if needed), nutrition, exercise, and targeted support—to create a comprehensive and personalized path forward.
Core Components of an Integrative ADHD Plan
| Strategy Area | Practical Examples | Potential Benefit for Brain Health |
|---|---|---|
| Medical Support | Working with a psychiatrist; considering stimulants or non-stimulants. | Helps correct neurotransmitter imbalances, improving focus and impulse control. |
| Brain-Fueling Nutrition | Meals rich in protein (eggs, lean meat) and complex carbs (whole grains, fruit). | Provides stable energy to the brain, avoiding sugar crashes that worsen inattention. |
| Physical Activity | Daily bike rides, playing tag, dancing, or team sports for 30-60 minutes. | Naturally boosts dopamine and norepinephrine, which improves mood and focus. |
| Targeted Supplements | High-quality Omega-3 fish oil (rich in EPA/DHA); checking for iron/zinc levels. | Supports brain cell structure and communication, potentially filling nutritional gaps. |
By weaving these strategies together, parents can build a robust support system that not only manages symptoms but also fosters long-term brain health and resilience for their child.
Disclaimer: The information provided in this article is for educational purposes only and is not intended to diagnose or treat any medical condition. Please consult with a qualified healthcare professional before making any decisions about medication, supplements, or significant lifestyle changes for your child.
A Responsible Guide to Supplements
While a solid foundation of a balanced diet and regular exercise is non-negotiable for any integrative ADHD plan, many parents understandably explore supplements for that extra layer of support. But this isn't about finding a magic bullet. It's about taking a responsible, evidence-based path to fill specific nutritional gaps.
Before you even think about adding a new supplement to your child's routine, the first step is always to talk with their healthcare provider. This is critical. They can help figure out if a supplement is actually needed, confirm it’s safe, and make sure it won’t interfere with any medications or other treatments your child is on.
Key Supplements for Brain Health
Certain nutrients are heavy hitters when it comes to brain function and the communication networks that support focus and emotional regulation. When you start looking at the options, it helps to know what they do and how to pick a good one.
Omega-3 Fatty Acids are probably the most-studied supplements for ADHD, and for good reason. These healthy fats, especially EPA (eicosapentaenoic acid) and DHA (docosahexaenoic acid), are the literal building blocks of brain cells.
- How to Choose: Look for a high-quality fish oil that’s been third-party tested for purity—this ensures it's free of heavy metals. Pay close attention to the EPA/DHA ratio on the label. Some research suggests that a higher concentration of EPA might be particularly helpful for focus. Affordable store brands often provide excellent, purified options.
Iron, Zinc, and Magnesium are essential minerals that play a huge role in producing neurotransmitters and supporting overall brain health. It's not uncommon for a deficiency in one of these to look a lot like ADHD symptoms, or even make existing symptoms of inattention and hyperactivity worse.
- Next Steps: Don't just guess. Ask your pediatrician about running a simple blood test to check for deficiencies. This takes the guesswork out of it and ensures you’re addressing a real, specific need instead of just adding more pills to the mix.
A supplement is meant to supplement a healthy lifestyle—not replace it. The biggest and most lasting changes almost always start on the plate with whole foods. Targeted, professional-guided supplementation comes second, only if it's truly needed.
Ultimately, using supplements responsibly means you're making informed decisions as a team with your child's doctor. This partnership ensures that anything you add to your child's routine is both safe and effective, supporting their well-being as one part of a complete, thoughtful strategy.
Building a Supportive Home Environment with Daily Routines
Beyond specific therapies or medications, creating a structured and predictable home environment is one of the most powerful tools you have to help a child with ADHD thrive. Consistency calms an anxious mind, reduces the daily friction of decision-making, and helps build those crucial executive function skills that are so often a challenge. The goal isn't rigidity; it's about creating a dependable rhythm for the day that makes life less overwhelming for everyone.
Getting started doesn't have to be complicated. You can make a huge impact by focusing on the most chaotic parts of the day: mornings and evenings. Simple visual aids like charts or checklists are incredibly effective because they externalize the steps for a task, taking the burden off your child's working memory.

Practical Steps for Building Structure
A supportive environment is all about breaking down big challenges into small, manageable actions. Instead of a vague (and overwhelming) command like, "Clean your room," try breaking it down into a clear sequence. "First, put your dirty clothes in the hamper. Then, put your books on the shelf."
Here are a few brain-healthy habits you can start implementing right away:
- Dedicated Workspace: Designate one specific, clutter-free spot just for homework. This simple act trains the brain to associate that location with focus.
- Screen Time Boundaries: Set clear, predictable limits on screen time. Unhealthy habits like unstructured digital consumption can make it much harder for the ADHD brain to regulate attention and transition to other activities.
- Prioritize Sleep Hygiene: A consistent bedtime, even on weekends, is non-negotiable. A well-rested brain is far better equipped to manage ADHD symptoms, whether they are inattentive or hyperactive. This simple daily habit is a cornerstone of mental health.
A predictable routine acts like an external scaffold for a child's developing executive functions. It reduces the sheer number of decisions they have to make, freeing up precious mental energy to focus on what’s important.
These daily habits do so much more than just manage behavior; they empower your child with a genuine sense of control and accomplishment. By building a foundation of consistency, you reduce household stress and provide the stability your child needs to flourish. For more actionable strategies, check out our 15 tips for supporting a child with ADHD.
Disclaimer: This information is for educational purposes and is not intended to diagnose or treat any medical condition. Always consult with a qualified healthcare professional before discussing medications, supplements, or making significant lifestyle changes.
Got Questions About ADHD vs. ADD? We've Got Answers.
As you start to understand the ins and outs of ADHD, it's natural for questions to pop up. It's a complex world, and the terminology alone can be confusing. Let’s tackle some of the most common things parents ask.
Is ADD Still a Thing?
The short answer is no. "ADD," or Attention Deficit Disorder, is actually an old, outdated term. Since 1994, the medical community has officially used Attention Deficit Hyperactivity Disorder (ADHD) to cover all presentations of the condition.
So what most people used to call ADD is now officially known as ADHD, Predominantly Inattentive Presentation. It’s just a more specific way of describing the same challenges with focus and attention.
What’s the Best Diet for a Kid with ADHD?
There’s no magic "ADHD diet," but focusing on brain-healthy foods can make a real difference. The goal is to keep your child's energy and blood sugar stable.
Think whole foods. Meals built around protein (like eggs and beans) and complex carbs (oatmeal, veggies) are fantastic for sustained focus. On the flip side, limiting unhealthy habits like consuming processed foods, sugary snacks, and artificial additives is one of the smartest moves you can make. Affordable options include buying produce in season and leaning on pantry staples like beans and whole grains.
Do Supplements Like Fish Oil Actually Work?
This is a big one. Omega-3 supplements, especially fish oil packed with EPA and DHA, are crucial for healthy brain cells. It's literally brain food. Some studies suggest a link between omega-3s and improved focus.
The key is quality. If you go this route, always choose a high-quality, third-party tested brand to ensure purity—affordable store brands are often a great choice. But first, have a conversation with your pediatrician or a specialist. They can help you figure out if it's the right move and even test for common nutritional deficiencies, like low iron or zinc, that can sometimes mimic attention problems.
How Can Exercise Help with ADHD Symptoms?
Never underestimate the power of movement. Exercise is one of the most effective, all-natural tools we have for managing ADHD symptoms and is a primary brain-healthy activity.
When your child runs, jumps, or plays, their brain naturally releases more dopamine and norepinephrine. These are the very same neurotransmitters that many ADHD medications target. Building a daily habit of fun physical activity can do wonders for focus, hyperactivity, and overall mood.
Disclaimer: This information is for educational purposes and is not intended to diagnose or treat any medical condition. Always consult with a qualified healthcare professional before discussing medications, supplements, or making significant lifestyle changes.
If you're seeking a clear diagnosis and a personalized, evidence-based plan for your child, the team at Children Psych is here to help. We provide comprehensive evaluations and compassionate care for families across California. Learn more about our approach and schedule a consultation today.