For parents of a child with bipolar disorder, the connection between mood and sleep isn't just a casual observation—it's one of the most critical parts of managing their well-being. Sleep problems aren't just a side effect of the condition; they are a core feature that can both predict and even trigger major mood episodes. This makes a holistic approach to sleep a powerful focus for creating stability.
Disclosure: This information is for educational purposes only and is not intended to diagnose or treat any medical condition. Please consult with a qualified healthcare professional before making any decisions about medications, supplements, or your child's health.
The Unbreakable Link Between Bipolar Disorder and Sleep
As a parent, you've probably seen it firsthand: your child's sleep patterns shift, and a change in their mood isn't far behind. This isn't just in your head—it’s a fundamental part of how bipolar disorder works in the brain. The relationship is a frustrating cycle where poor sleep worsens mood instability, and mood episodes completely wreck sleep. Understanding this two-way street is the first step toward building effective, supportive strategies at home.
Sleep disturbances are one of the most common hurdles for kids and teens with bipolar disorder. Research shows just how widespread the problem is. One study found that 40% of patients deal with insomnia, while another 29% struggle with hypersomnia (excessive sleeping). During acute manic episodes, the numbers are even more dramatic, with 69% to 99% of patients experiencing a drastically reduced need for sleep. You can learn more about how mental illness and lack of sleep are connected in our deep-dive article on the topic.
How Bipolar Mood States Affect Your Child's Sleep
Learning to spot the specific ways sleep changes during different mood states is like getting an early warning system. Each phase of bipolar disorder brings its own unique sleep signature. This table gives you a quick overview of what to look for.
| How Bipolar Mood States Affect Your Child's Sleep | |
|---|---|
| Mood State | Typical Sleep Changes |
| Mania | A sudden, dramatic drop in the need for sleep is a classic sign. They might sleep only 2-3 hours but wake up feeling incredibly energetic and wired, as if they’d slept a full night. |
| Hypomania | The need for sleep decreases, but not as severely as in full mania. They might start staying up later, waking up earlier, and still feel more productive or energized than usual. |
| Depression | This state often brings hypersomnia, or excessive sleeping. Your child might sleep 10+ hours a night and still feel exhausted, struggling to get out of bed. Insomnia can also occur, where they can't fall or stay asleep despite feeling tired. |
| Mixed State | Sleep becomes chaotic and unpredictable. They might have the racing thoughts and energy of mania ("tired but wired") while also feeling the deep fatigue and despair of depression, making restful sleep feel impossible. |
| Euthymia (Stable Mood) | Sleep patterns become more regular and predictable. Even during these stable periods, maintaining a consistent sleep schedule is one of the most important things you can do to prevent a future mood episode. |
A child in a manic or hypomanic state might suddenly claim they only need a few hours of sleep yet wake up with boundless energy. On the flip side, a depressive episode often brings an overwhelming fatigue that makes getting out of bed feel impossible, even after sleeping for ten hours or more. That's why even during stable periods, a structured sleep schedule becomes a non-negotiable pillar of their management plan.
"Managing sleep is arguably the single most effective thing people can do to increase their quality of life with bipolar disorder. It's not just about feeling rested; it's about regulating the brain's very chemistry."
This guide will walk you through an integrative approach to support your child's brain health, combining practical daily habits with the roles of diet, exercise, and medication. Our goal is to empower you with the knowledge and tools you need to create a more stable and predictable world for your child.
Disclosure: This article is for educational purposes only. Please consult a qualified healthcare professional for diagnosis, treatment, and before making any changes to your child's medication or supplement regimen.
Why Sleep Is a Powerful Lever for Mood Stability
To get a real sense of the powerful link between sleep and bipolar disorder, it helps to picture your child's brain as a finely tuned orchestra. This complex orchestra is supposed to be led by a conductor called the circadian rhythm—the body's internal 24-hour clock that keeps everything from hormones to mood playing in harmony. But in a child with bipolar disorder, that conductor is often dysregulated, throwing the entire orchestra out of sync.
When the circadian rhythm is off-key, it messes with the release of crucial brain chemicals like serotonin and dopamine, the very neurotransmitters that regulate mood. An unstable internal clock creates a cascade of problems, where even one night of poor sleep can be enough to trigger a major mood shift.
This diagram shows how different mood states in bipolar disorder are directly tied to distinct sleep patterns.
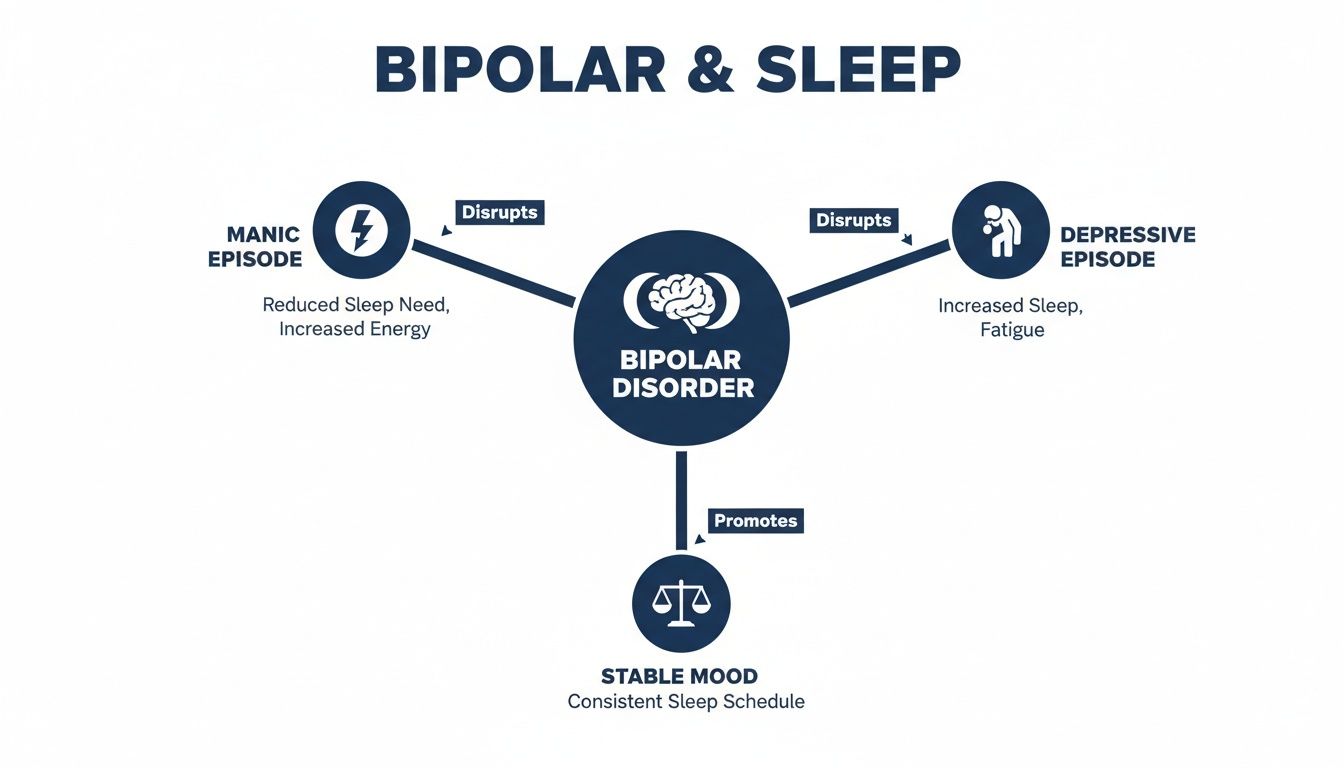
As you can see, mania, depression, and stability each create a unique sleep signature. This is exactly why tracking sleep is such a vital tool for monitoring your child's well-being.
The Science Behind Sleep and Mood
The connection goes much deeper than just feeling tired. We now know that sleep deprivation can actually activate specific genes linked to manic episodes. It’s like flipping a switch in the brain that pushes it toward an elevated state. This is why a consistent sleep schedule isn't just a "good habit"—it's a form of biological intervention. By stabilizing sleep, you are helping to retune your child's brain chemistry at a fundamental level.
Think of it this way: a stable sleep routine acts as an anchor for the circadian rhythm. When your child goes to bed and wakes up around the same time every single day, it gives their internal conductor a steady beat to follow. That predictability helps their neurotransmitter systems function correctly, making mood episodes far less likely to take hold.
The Role of an Integrative Approach
This is where an integrative approach becomes so essential. It recognizes that brain health isn't supported by just one thing, but by a combination of healthy habits working together in concert.
- Brain-Healthy Diet: Certain nutritional gaps can make sleep and mood issues worse. Making sure your child gets enough magnesium (found in leafy greens) and omega-3s (from fish) can support calmer brain function. Affordable options like canned salmon, flax seeds, and spinach can make a real difference.
- Daily Exercise: Physical activity is one of the best things you can do for the brain. A daily 30-minute walk or bike ride, especially in the morning, helps reset the circadian clock and burns off the anxious energy that often keeps kids up at night.
- Supplement Support: When diet alone isn't cutting it, supplements can help fill in the gaps. Omega-3 supplements, especially those with a higher ratio of EPA to DHA, have been shown to support mood. When choosing one, look for third-party testing seals (like USP or NSF) to ensure quality. And, of course, always talk to a healthcare professional before starting any new supplement.
How Medication Fits In
For many families, psychotropic medications are a critical piece of the puzzle. Mood stabilizers and other medications work by directly targeting the brain's overactive or underactive signaling pathways. They can help regulate neurotransmitter function, calming the biological storm that disrupts sleep and drives mood swings.
By quieting the racing thoughts of mania or lifting the heavy fog of depression, medication can create the necessary brain stability that allows healthy habits, like a consistent sleep schedule, to be truly effective.
This is why combining medication with strong daily routines—consistent sleep, a balanced diet, and regular exercise—creates such a powerful effect. The medication provides the biological foundation for stability, and the healthy habits reinforce it, day in and day out.
Disclaimer: The information in this article is intended for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always consult with a qualified healthcare professional before making any decisions about your child's health, medications, or supplements.
Your Integrative Toolkit for Better Sleep
Managing the intricate dance between bipolar disorder and sleep calls for more than just a single solution. It requires a multi-faceted strategy, one that supports your child's brain from every possible angle. Think of it as assembling a toolkit focused on the foundational pillars of brain health: diet, exercise, and targeted supplements. By weaving these elements into your child's daily life, you create a powerful support system that fosters mood stability and invites restorative rest.

This isn’t about finding a magic bullet. Instead, it’s about making small, consistent changes that build on one another, creating a ripple effect of positive impact. Each piece of the toolkit works with the others to help regulate your child's internal clock and soothe their nervous system, making it easier for them to get the deep, healing sleep their brain desperately needs.
Fueling the Brain with a Nutrient-Dense Diet
What your child eats has a direct line to their brain chemistry and, by extension, their ability to sleep. A brain-healthy diet doesn’t have to be complicated or break the bank. It really boils down to adding more whole, nutrient-packed foods while dialing back on things that trigger inflammation or throw sleep cycles out of whack.
Many common habits, like reaching for sugary snacks or relying on processed meals, can send blood sugar on a rollercoaster ride of spikes and crashes that messes with both mood and sleep. These foods are also often missing the key micronutrients the brain needs to produce calming neurotransmitters.
Here are some affordable, brain-friendly food groups to start weaving into your meals:
- Omega-3 Fatty Acids: Absolutely essential for brain cell structure and tamping down inflammation. You can find these in affordable sources like canned salmon, sardines, flax seeds, and chia seeds.
- Magnesium-Rich Foods: This mineral is a superstar for calming the nervous system. It’s abundant in leafy greens like spinach, plus almonds, black beans, and bananas.
- Complex Carbohydrates: Foods like oats, brown rice, and sweet potatoes offer a slow, steady release of energy and help promote serotonin, a key player in the sleep process.
A simple daily habit could be adding a tablespoon of ground flaxseed to their morning oatmeal or including a side of spinach with dinner. These small additions accumulate over time to correct potential nutritional deficiencies that can impact mood and sleep.
Exercise as a Primary Brain-Healthy Activity
When you start to see exercise as a brain health activity—not just a physical one—its importance clicks into place. Physical activity is one of the most powerful non-medical tools we have for regulating circadian rhythms and burning off the anxious energy that so often fuels insomnia.
Regular movement helps reset the body's internal clock, especially when it’s done in the morning with a dose of natural light. It also helps metabolize the stress hormone cortisol and boosts feel-good endorphins, which can help lift the depressive symptoms that lead to oversleeping.
Think about easy-to-implement daily habits:
- A 20-30 minute family walk after dinner.
- A bike ride around the block before homework starts.
- Putting on some favorite music for a quick 15-minute dance party.
The real goal here is consistency, not intensity. A short, daily burst of activity is far more beneficial for regulating the bipolar and sleep cycle than hitting the gym hard once or twice a week.
Understanding the Role of Supplements
While getting nutrients from food is always the best first step, supplements can be a practical way to fill in nutritional gaps that are tough to cover through diet alone. But it's critical to choose wisely and always talk with a healthcare professional before adding anything new to your child's routine.
When looking at supplements, quality and bioavailability are everything. Look for third-party certifications (like USP or NSF) on the label. This is your assurance that the product actually contains what it says it does, without any harmful extras.
Here are three key supplements known to support brain health and sleep:
- Omega-3s: Find a supplement with a higher ratio of EPA (eicosapentaenoic acid) to DHA. EPA has stronger links to mood-regulating benefits. A high-quality, purified fish oil is a great choice, or an algae-based oil if you need a vegan option.
- Magnesium Glycinate: This form of magnesium is easily absorbed by the body and is well-known for its calming effect on the brain. It’s particularly great for promoting sleep without causing the digestive issues some other forms of magnesium can.
- Vitamin D: Often called the "sunshine vitamin," Vitamin D is vital for mood regulation. A surprising number of children are deficient, especially during the darker winter months.
How Medication Supports the Integrative Model
For many, psychotropic medications are the bedrock of treatment. They work to stabilize brain chemistry in a way that lifestyle changes alone just can't. Think of medication as the stable foundation upon which all these other integrative strategies—diet, exercise, supplements—can be successfully built.
Different types of medications play distinct roles:
- Mood Stabilizers: These work to smooth out the extreme highs and lows, preventing the neurochemical chaos that wrecks sleep.
- Atypical Antipsychotics: While often used for their mood-stabilizing effects, they can also be incredibly helpful for quieting the racing thoughts of mania that make sleep feel impossible.
- Antidepressants: When prescribed carefully by a psychiatrist (often alongside a mood stabilizer), they can lift the heavy blanket of depressive fatigue and help normalize sleep patterns.
By addressing the underlying biological imbalances, these medications can create the calm and stability your child needs to truly benefit from healthy habits like a consistent diet, regular exercise, and a solid sleep routine.
The connection between sleep and well-being in bipolar disorder is not just anecdotal; it's profound. Research clearly shows that as sleep quality goes down, so does a person's quality of life. This isn't a small dip—it's a sharp decline in their ability to function and find satisfaction. You can discover more insights about these findings on sleep's impact from the study. This science is exactly why a comprehensive, integrative approach that includes medication, diet, and lifestyle is so vital.
Disclaimer: This information is for educational purposes and is not intended to diagnose or treat any medical condition. Always consult with a qualified healthcare professional before starting any medications or supplements.
Crafting a Calming and Predictable Evening Routine
For a child or teen with bipolar disorder, a consistent evening routine is so much more than a simple checklist of habits. Think of it as a powerful, non-verbal signal to their brain that it’s time to shift gears from the day's activity to the quiet of the night. An erratic evening schedule can send mixed messages to an already dysregulated internal clock, turning the transition to sleep into a nightly battle.
By creating a predictable sequence of events, you help anchor their circadian rhythm, making it much easier for both their mind and body to wind down.

The first step is to spot and gently reduce the habits that are sabotaging sleep. These activities often overstimulate the brain right when it needs to be calming down, pouring fuel on the fire of bipolar and sleep challenges. The goal isn't perfection, but consistent, gentle reduction of these disruptions.
Unhealthy Habits to Gently Reduce
Screen time is one of the biggest culprits here. The blue light blasting from phones, tablets, and computers is particularly disruptive because it actively suppresses the brain's production of melatonin—the hormone that says, "Hey, it's time to get sleepy." You can learn more about the mental health risks tied to excessive screen time and lack of exercise in our deep-dive guide.
Here are a few key habits to start dialing back:
- Late-Night Screen Use: This isn't just about blue light. Video games, social media scrolling, and intense TV shows are designed to be stimulating, often triggering the racing thoughts that keep kids awake.
- Intense Exercise or Activities: A hard workout or a competitive game too close to bedtime can jack up cortisol and adrenaline levels, making it nearly impossible for the body to relax.
- Heavy Meals or Sugary Snacks: A big meal can lead to digestive discomfort that keeps them up. Sugary foods are even worse, causing a blood sugar spike followed by a crash that can fragment sleep all night long.
A Blueprint for a Brain-Healthy Wind-Down
Once you start chipping away at the stimulating habits, you can fill that time with calming, brain-healthy activities. The real magic is in creating a sequence that's both soothing and repeatable, night after night. That consistency is what trains the brain to recognize the cues for sleep.
A predictable evening routine acts as a gentle, non-verbal cue to a child's nervous system. It communicates safety, predictability, and calm, helping to quiet the racing thoughts that so often keep them awake.
Here are some practical, affordable ideas to build into your child's routine:
- Establish a 'Tech Curfew': This is non-negotiable. Set a firm rule that all screens are turned off at least 60-90 minutes before bedtime. This gives melatonin levels a chance to rise naturally. Have devices charge outside the bedroom to eliminate temptation.
- Take a Warm Bath: Adding Epsom salts (a great source of magnesium) to a warm bath can help relax tense muscles and soothe the nervous system. The drop in body temperature after they get out also naturally triggers sleepiness.
- Engage in Quiet Activities: Swap the screen for a physical book, an audiobook, or some calming music. Gentle stretching or drawing also works wonders to slow the mind without the disruptive blue light.
- Practice 'Brain Dumping': For a child whose mind won't shut off, journaling can be a game-changer. Encourage them to write down any worries, thoughts, or to-do lists from the day. This simple act gets the thoughts out of their head and onto paper, making it easier to let go.
Below is a sample schedule you can adapt. Remember, the specific activities matter less than the consistency. Find what works for your child and stick with it.
| Sample Evening Wind-Down Schedule | |
|---|---|
| Time | Activity |
| 7:30 PM | Tech Curfew Begins. All screens (phones, tablets, TV) are turned off and put away for the night. |
| 7:45 PM | Prepare for Tomorrow. Lay out clothes and pack the school bag to reduce morning stress. |
| 8:00 PM | Warm Bath or Shower. Use this time to relax muscles and begin the calming process. |
| 8:30 PM | Quiet Activity. Read a chapter of a book, listen to a calming playlist, or do some light stretching. |
| 8:45 PM | Journaling / Brain Dump. Spend 5-10 minutes writing down thoughts or worries from the day. |
| 9:00 PM | Lights Out. The bedroom should be cool, dark, and quiet to create an ideal sleep environment. |
How Medication Can Help Stabilize Sleep and Mood
For many families navigating pediatric bipolar disorder, medication is an essential piece of the puzzle. It creates the biological stability that allows all the other strategies—like therapy and healthy routines—to actually take root and work. For parents, understanding how these medications can help can clear up a lot of the fear and uncertainty around them, showing how they can restore a sense of calm to a child’s brain and their sleep cycle.
Think of the brain during a manic or depressive episode as being stuck in a biological storm. Psychotropic medications work by helping to regulate the brain's delicate neurochemistry, essentially calming that storm so your child can find their footing again.
The Role of Different Medications
Medications provide a foundation of stability, making it possible for your child to engage with and benefit from the healthy sleep routines and therapies we’ve discussed. Different types of medication target specific brain functions to bring things back into balance.
- Mood Stabilizers: These are often the cornerstone of treatment. Just as the name suggests, they work to even out the intense highs and debilitating lows, preventing the kind of extreme brain activity that completely hijacks sleep. By balancing neurotransmitters, they improve the brain’s potential for consistent rest.
- Atypical Antipsychotics: These can be incredibly helpful for quieting the racing thoughts and mental "static" that are so common in mania. When a child's mind is going a mile a minute, sleep feels impossible. These medications can reduce that noise, allowing the brain to finally transition into a restful state and improving focus during the day.
- Antidepressants: When used carefully and always under the close watch of a child psychiatrist—often alongside a mood stabilizer—these can lift the heavy fog of depression. This can be key for normalizing sleep, especially for a child who is dealing with hypersomnia (excessive sleeping) and struggling with motivation. By improving mood, these medications enhance the brain's ability to regulate sleep-wake cycles.
Creating a Powerful Partnership: Meds and Habits
Medication doesn't work in a vacuum. Its true power is unlocked when it’s combined with the consistent, healthy habits that build resilience. When medication helps stabilize the brain's internal chemistry, it suddenly becomes so much easier for a child to stick to a sleep schedule, eat nourishing meals, and get regular exercise.
This creates a powerful synergistic effect where biology and behavior support each other. Medication lays the groundwork for stability, which in turn empowers your child to practice healthy routines. Those routines then reinforce the brain’s stability, making the medication even more effective. This positive feedback loop is a key reason why consistent psychiatric medication management is so critical for long-term success.
The link between bipolar disorder and sleep disruption is not just anecdotal; it's incredibly well-documented. Global data shows that sleep disorder symptoms affect between 41% and 52% of people with bipolar disorder. During active mood episodes, that number skyrockets to over 60%. One analysis even revealed that 70% of patients experienced some form of sleep disruption. You can read the full research about these bipolar and sleep findings to get a deeper sense of the scale of this issue.
By directly addressing the neurobiological roots of mood episodes, medication can significantly improve your child's brain function, making restorative sleep possible and enhancing their potential for long-term mental wellness.
Ultimately, finding the right medication or combination of medications is a careful, collaborative process. Working closely with an experienced child psychiatrist allows for thoughtful adjustments to find the most effective treatment with the fewest side effects, giving your child the best possible support on their journey to wellness.
Disclaimer: This information is for educational purposes only and is not intended to be a substitute for professional medical advice. Always consult a qualified healthcare professional before making decisions about medications or supplements for your child.
Navigating Next Steps and Seeking Professional Support
While building solid routines, a brain-healthy diet, and regular exercise are the bedrock of stability, sometimes they just aren't enough. The intricate dance between bipolar disorder and sleep can be incredibly complex, and knowing when to escalate your concerns is one of the most important things you can do for your child.
Always, always trust your gut. If something feels off, it probably is. Seeking an expert opinion is never the wrong decision—it’s a powerful act of advocacy.
There comes a point when a comprehensive psychiatric evaluation is the necessary next step. We’re not talking about minor sleep hiccups here. We’re talking about significant shifts that signal a deeper level of dysregulation that needs a professional eye.
When to Seek a Professional Evaluation
So, when have you crossed the line from manageable home strategies to needing professional backup? Here are a few clear patterns that tell you it's time to make that call:
- Persistent Sleep Loss: Your child is getting only a few hours of sleep for several nights in a row, and there’s no obvious reason for it (like a sleepover or a big exam).
- Dramatic Mood and Sleep Shifts: You see a sudden, sharp decrease in the need for sleep that’s paired with classic manic symptoms like high energy, intense irritability, or racing thoughts. On the flip side, you might see a sudden swing to excessive sleeping coupled with deep sadness, hopelessness, or social withdrawal.
- Safety Concerns: This one is non-negotiable. If any sleep disturbance is connected to talk of self-harm, suicidal thoughts, or intense hopelessness, you need to get immediate professional help.
An expert evaluation is the only way to get a clear, accurate diagnosis. A child and adolescent psychiatrist is trained to tell the difference between bipolar-related sleep issues and other conditions like primary insomnia, anxiety disorders, or ADHD. Getting the diagnosis right is critical for creating a treatment plan that actually works. This assessment becomes the blueprint for a personalized, evidence-based strategy that combines behavioral tools with medical support.
Seeking a professional evaluation is not a sign of failure. It is a proactive step toward getting your child the precise support their unique brain chemistry needs. It opens the door to a targeted treatment plan that can restore stability.
Connecting with specialists is also easier than ever. With the rise of telehealth, your family can get expert care right from your own home, cutting out the stress of travel and long wait times. The most important message to take away is this: act on your concerns without delay. Reaching out for professional guidance is the most powerful next step you can take.
Disclosure: This article is for educational purposes only and is not intended to diagnose or treat any medical condition. Please consult a qualified healthcare professional for diagnosis, treatment, and before making any changes to your child's medication or supplement regimen.
Got Questions About Bipolar Disorder and Sleep?
When you're trying to manage the tangled relationship between your child's bipolar disorder and their sleep, a lot of questions come up. Let's tackle some of the most common ones parents ask.
Can We Just Fix My Child's Sleep with Diet and Exercise?
A brain-healthy diet and regular exercise are absolutely crucial. Think of them as the foundation you build everything else on—they can make a huge difference in mood stability and sleep quality.
But they work best as part of a bigger, more complete plan. Bipolar disorder is a complex brain condition that usually needs a combination of approaches: solid routines, therapy, and often medication. Diet and exercise are powerful allies that help all the other treatments work better. For example, getting outside for some physical activity helps reset the body's internal clock, and cutting back on sugar helps you dodge those late-night blood sugar crashes that wreck sleep.
How Can I Tell If My Teen Is Manic or Just a Typical Night Owl?
This is a big one. The key difference comes down to the need for sleep versus the desire for it. A neurotypical teenager might choose to stay up late texting friends and then drag themselves out of bed the next morning, feeling exhausted.
A teen heading into a manic or hypomanic episode feels like they don't need to sleep. They might be up until 3 a.m. full of energy, sleep for just a couple of hours, and then wake up feeling fantastic and ready to take on the world. If you see a sharp drop in their sleep time combined with a huge surge in energy, racing thoughts, or impulsive behavior, that's a major red flag to call a professional.
A reduced need for sleep isn't just a preference for a later bedtime; it's a hallmark sign of mania. It signals a deep biological shift in the brain's fundamental drive for rest.
Are Over-the-Counter Sleep Aids Like Melatonin Okay to Use?
You should never give a child or teen with bipolar disorder any over-the-counter sleep aids—including melatonin—without getting a direct green light from their psychiatrist first. It’s just not worth the risk.
Supplements and OTC products can have completely unpredictable effects on a brain that's already sensitive. Some can destabilize mood or, in the worst-case scenario, even help trigger a manic episode. A qualified professional can point you toward safe, targeted options that are a good fit for your child's unique brain chemistry and overall treatment plan, whether that's a specific form of magnesium or another carefully chosen supplement.
At Children Psych, we know that figuring out your child's mental health is a journey, and you don't have to walk it alone. Our team of expert child and adolescent psychiatrists is here to provide compassionate, evidence-based care that brings together therapy, medication management, and lifestyle support to help your child truly thrive. To learn more about how we can help, or to schedule a consultation, please visit us at https://childrenpsych.com.