If you’ve heard people use both "ADD" and "ADHD," you're not alone. It’s a common point of confusion for parents, but the core difference is simple: ADD is an outdated term. The symptoms people once called ADD are now officially known as Attention-Deficit/Hyperactivity Disorder (ADHD), Predominantly Inattentive Presentation.
In short, the medical community updated the name to better reflect the condition's complexity. They recognized that attention challenges don’t always come with hyperactivity, but they are all part of the same underlying neurodevelopmental condition.
Understanding the Shift From ADD to ADHD

So, why the change? Back in 1994, the American Psychiatric Association officially consolidated all related attention disorders under the single diagnosis of ADHD. This was a deliberate move to show that inattention, hyperactivity, and impulsivity are all related components of the same disorder, even if one set of symptoms is more obvious than another in a particular child.
Today, instead of just "ADHD," a diagnosis will specify one of three presentations. This gives professionals and parents a much clearer picture of a child’s unique struggles.
- ADHD, Predominantly Inattentive Presentation: This is the modern term for what was once called ADD. It’s defined by challenges with focus, organization, and seeing tasks through to completion, without major signs of hyperactivity.
- ADHD, Predominantly Hyperactive-Impulsive Presentation: This presentation is characterized by restlessness, an inability to sit still, constant fidgeting, and acting on impulse without thinking things through.
- ADHD, Combined Presentation: As the name suggests, a child with this presentation shows a significant mix of both inattentive and hyperactive-impulsive symptoms.
Quick Guide From ADD to the Three Types of ADHD
To clear up any lingering confusion, this table breaks down how the old term fits into today's diagnostic framework.
| Old Term | Current ADHD Presentation | Core Symptoms |
|---|---|---|
| ADD (Attention Deficit Disorder) | ADHD, Predominantly Inattentive Presentation | Difficulty focusing, disorganization, forgetfulness. |
| N/A | ADHD, Predominantly Hyperactive-Impulsive Presentation | Fidgeting, excessive talking, inability to wait, impulsivity. |
| N/A | ADHD, Combined Presentation | A significant number of symptoms from both categories. |
Understanding this evolution helps you advocate for your child with clarity and precision. It moves the conversation beyond an outdated label and toward a specific diagnosis that guides a truly effective support plan.
A Modern, Integrative View of Management
Knowing your child's specific ADHD presentation is the first step toward building a successful, integrative treatment plan. A modern, holistic approach looks at the whole child, combining proven medical treatments with supportive lifestyle strategies.
For example, psychotropic medications like stimulants or non-stimulants are powerful tools that can be incredibly effective. They work on key neural pathways in the brain to improve focus, reduce impulsivity, and help a child better regulate their emotions and actions. By balancing brain chemistry, these medications can unlock a child's potential to learn and thrive.
For many families, this is one important piece of a larger puzzle. A comprehensive plan also incorporates a brain-healthy diet, targeted supplements, regular exercise, and healthy daily habits to support the brain and body from every angle.
Key Takeaway for Parents: Thinking about your child's needs through the lens of the three ADHD presentations allows for a more personalized, integrative approach that combines medical support with practical, everyday strategies for success.
For a deeper dive into the condition itself, you might find our guide on what ADHD is in children helpful.
Disclaimer: This information is for educational purposes only and is not intended to diagnose or treat any medical condition. Please consult with a qualified healthcare professional before making any decisions about medications, supplements, or treatment plans for your child.
Recognizing the Three Presentations of ADHD in Your Child
Knowing the official terminology is one thing, but seeing how ADHD actually shows up in your child’s daily life is what really matters. The main difference between what we used to call ADD and today’s broader understanding of ADHD comes down to recognizing how inattentive and hyperactive-impulsive symptoms appear. These behaviors aren't signs of a bad attitude or laziness; they’re just expressions of how your child's brain is wired.
Spotting these patterns is the first real step toward creating a supportive, integrative plan that fits your child’s unique needs. Often, the best results come from a holistic approach that blends conventional treatments with practical, easily implemented lifestyle adjustments.
The Predominantly Inattentive Child (Formerly ADD)
This is often the quietest presentation and can be easily missed, especially in girls. A child with inattentive ADHD might seem like a daydreamer, totally lost in their own world. You might give them a simple instruction like, "please go upstairs and get your shoes," only to find them minutes later completely sidetracked by a toy, the request long forgotten.
They might constantly misplace homework, lose their jacket at school, or have a really hard time following multi-step directions. Teachers may even describe them as "unmotivated" because they don't finish assignments, even when they understand the material perfectly. For a deeper dive, check out our guide on the symptoms of ADHD and available medications.
The Predominantly Hyperactive-Impulsive Child
This presentation tends to be much more obvious. A child with hyperactive-impulsive ADHD seems to have an engine that just won't quit. They might find it nearly impossible to stay in their seat during dinner, constantly squirming, fidgeting, or just getting up to run around the room.
Impulsivity is the other major piece of the puzzle. This can look like interrupting others, blurting out answers in class before they're called on, or struggling to wait their turn in games. They often act without thinking through the consequences, which can lead to social friction or even accidental injuries.
The Combined Presentation Child
Many kids show a mix of both inattentive and hyperactive-impulsive symptoms. This is the child who can sit completely still for a video game they love (hyperfocus) but can't stay tuned in during a classroom lecture for more than a few minutes. They might remember every single detail of a favorite movie but forget to bring home their homework every single day.
These children are navigating a complicated inner world, battling restlessness and an inability to organize their thoughts at the same time. It can be incredibly frustrating for them because they genuinely want to do well but feel like their own brain is working against them.
Globally, ADHD diagnosis rates have climbed, but there’s a critical difference in how symptoms appear across genders. In the U.S., 11.4% of children have been diagnosed, with boys at 14.5% compared to girls. This gap often happens because hyperactivity in boys is easy to spot, while the quieter, inattentive symptoms more common in girls get overlooked, delaying crucial support. You can read more about these trends and gender differences in diagnosis.
An Integrative Path Forward
No matter the presentation, a supportive plan can make all the difference. Psychotropic medications, such as stimulants or non-stimulants, can be highly effective. These medications help improve communication between different parts of the brain, boosting focus, taming impulsivity, and unlocking a child's ability to learn and thrive.
Alongside medical support, a few simple daily habits can create a strong foundation for success:
- Brain-Healthy Diet: Start the day with protein-rich, affordable breakfasts like eggs or Greek yogurt to help stabilize energy and focus. Cutting back on processed foods, artificial dyes, and sugar can also minimize mood swings and improve concentration.
- Regular Exercise: Physical activity is one of the most powerful tools for brain health. A daily 30-minute session of running, biking, or even just dancing in the living room can improve concentration and burn off excess energy.
- Omega-3 Supplements: Fatty acids like EPA and DHA are essential for brain function. Look for affordable, high-quality fish oil supplements that have been third-party tested for purity. Always consult with a healthcare professional before starting any new regimen to discuss the right choice and dosage for your child.
By recognizing your child’s specific challenges and building a supportive, multi-faceted plan, you can empower them to navigate their world with far more confidence and success.
How Professionals Approach an ADHD Diagnosis
If you suspect your child might have ADHD, understanding how a diagnosis is actually made can bring some much-needed clarity. A proper evaluation isn't just about ticking boxes on a quick checklist; it’s a careful and detailed process where a professional gathers information from multiple sources to get the full picture.
The journey starts with a deep-dive clinical interview with both you and your child. This isn't just a casual chat. The clinician will ask about your child’s developmental history, your family's medical background, and the specific behaviors you've been seeing at home and in school. They’ll also talk directly with your child to hear about their own experiences and struggles.
Next up are standardized behavior rating scales. These are typically questionnaires given to parents, teachers, and sometimes other adults in your child’s life. This step is critical because it helps the clinician see if the challenging behaviors are showing up consistently across different environments—a key requirement for a diagnosis.
Using the DSM-5 Framework
To formalize the diagnosis, clinicians turn to the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5). Think of it as the official guidebook for diagnosing mental health conditions.
The DSM-5 lays out very specific symptoms for both inattention and hyperactivity/impulsivity. For a diagnosis, a child needs to show a certain number of these symptoms for at least six months, and these behaviors have to be more pronounced than what's typical for their age.
The infographic below breaks down the three presentations of ADHD as defined by the DSM-5. It’s a great visual for understanding the difference between what people used to call ADD and how we understand the condition today.
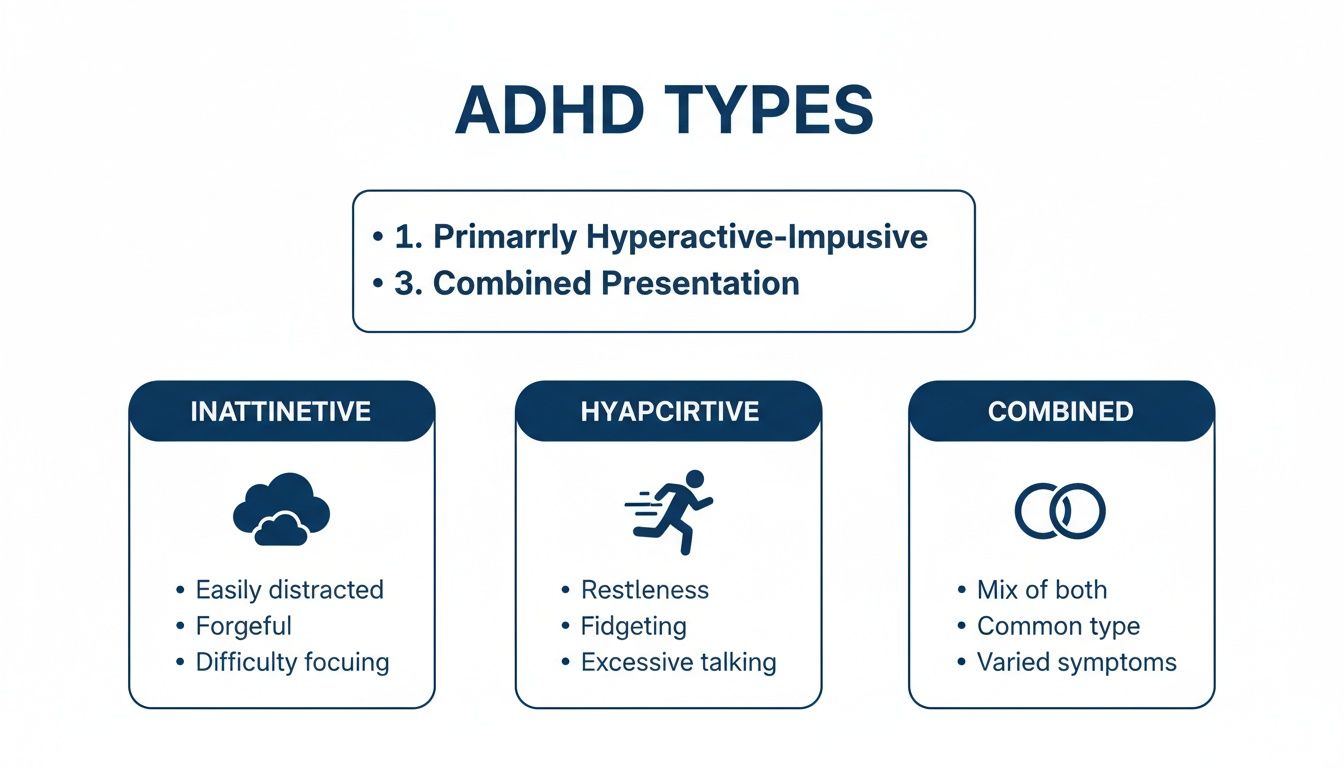
This guide helps parents quickly see how inattentive symptoms (what was once called ADD) are different from the hyperactive or combined types. This is really important for understanding the specific diagnosis your child receives and what it means for them.
Ruling Out Other Conditions
A huge part of a reliable diagnosis is what’s called differential diagnosis. The truth is, many other conditions can look a lot like ADHD.
A skilled clinician will carefully investigate and rule out other possibilities to make sure ADHD is the right diagnosis. Common mimics include:
- Anxiety disorders
- Learning disabilities
- Trauma
- Sleep disorders
- Even hearing or vision problems
This might involve more specialized testing to get a clearer view of your child’s cognitive abilities, helping pinpoint the real source of their difficulties. You can learn more by reading our guide on navigating an ADHD diagnosis online and what parents need to know.
A reliable ADHD diagnosis is never rushed. It is a meticulous, evidence-based process that looks at the whole child, empowering parents with the confidence to move forward with an effective and supportive plan.
This thorough evaluation ensures that any treatment plan—whether it involves therapy, medication, or lifestyle adjustments—is perfectly suited to your child's unique needs.
Disclaimer: This information is for educational purposes only and is not intended to diagnose or treat any medical condition. Please consult with a qualified healthcare professional before making any decisions about medications, supplements, or treatment plans for your child.
Building an Integrative ADHD Management Plan

When we build a truly successful ADHD management plan, we have to look at the whole child, not just a list of symptoms. The most effective approach is often an integrative one, which blends the best of conventional medicine with supportive lifestyle strategies to help your child thrive.
This balanced, holistic plan recognizes the very real, biological basis of ADHD while also empowering your family with practical, everyday tools. It’s all about supporting the brain directly, combining medical treatments with a strong foundation of healthy habits.
The Role of Psychotropic Medications
For many families, medication is a critical piece of the puzzle. It's important to understand that these medications aren't a "cure." Instead, they are powerful tools that help regulate brain chemistry, making it easier for a child to tap into their full potential. They work by improving how nerve cells communicate, which can sharpen focus and dial down impulsivity.
There are two main groups of psychotropic medications prescribed for ADHD:
- Stimulants: This is the most common group of medications. They work by increasing the levels of key brain chemicals called neurotransmitters, primarily dopamine and norepinephrine. This boost helps improve the brain's executive functions, leading to better attention, impulse control, and organization.
- Non-Stimulants: This group of medications works differently, often by targeting norepinephrine more gradually. They can be a great option for children who do not respond well to stimulants or experience side effects, providing a smoother, more sustained improvement in focus and emotional regulation.
By helping to balance brain function, these medications can create a neurological landscape where a child is better equipped to learn, manage their behavior, and connect with others. Any decision about medication must be made in close consultation with a qualified healthcare professional who can oversee the process.
Nutritional Support for Brain Health
You've probably heard it before, but it's true: what your child eats directly impacts their brain function and mood. An integrative plan puts a strong emphasis on a diet packed with brain-boosting nutrients and looks to correct common nutritional deficiencies that can worsen ADHD symptoms.
Here are a few simple but powerful nutritional strategies:
- Prioritize Protein: A breakfast loaded with protein—think affordable options like eggs, Greek yogurt, or a smoothie with protein powder—is a game-changer. Protein helps keep blood sugar stable and provides the raw materials for neurotransmitters, improving focus throughout the school day.
- Address Deficiencies: Research suggests children with ADHD may be more prone to low levels of certain minerals. Adding affordable foods rich in iron (lean meats, beans), zinc (pumpkin seeds, lentils), and magnesium (leafy greens, bananas) can be a big help. A healthcare provider can help determine if supplements are needed.
An integrative plan doesn’t have to be complicated or expensive. Simple swaps, like replacing a sugary cereal with scrambled eggs or adding a handful of pumpkin seeds to an afternoon snack, can make a significant difference in your child's ability to concentrate and regulate their energy.
The Impact of Unhealthy Habits
In our modern world, it’s all too easy for unhealthy habits to creep in, and for kids with ADHD, the effects can be magnified. Poor sleep and too much screen time are two of the biggest culprits that can undermine even the best-laid treatment plan.
An inconsistent bedtime or poor-quality sleep can actually mimic or worsen ADHD symptoms, leading to more irritability, inattention, and hyperactivity. Likewise, excessive screen time can overstimulate a developing brain, making it that much harder for a child to focus on less exciting (but necessary) tasks like homework.
Creating a supportive home environment means setting clear, consistent boundaries. This might look like a "no screens an hour before bed" rule or making sure your child gets at least 30-60 minutes of active play every single day to promote better sleep and focus.
Brain-Healthy Activities and Exercise
Never underestimate the power of movement. Exercise is one of the most effective non-medical tools we have for managing ADHD symptoms. Physical activity gets more blood flowing to the brain and boosts levels of dopamine and norepinephrine—much like stimulant medications do.
Making exercise a daily habit is a cornerstone of an integrative plan. This doesn’t have to mean organized sports or a trip to the gym. It can be as simple as:
- A brisk walk or bike ride after school.
- A spontaneous dance party in the living room.
- Jumping on a trampoline in the backyard.
These brain-healthy activities don’t just burn off extra energy; they also improve mood, sharpen focus, and pave the way for a better night's sleep. By weaving together medical support with these intentional lifestyle choices, parents can create a robust, well-rounded plan that truly helps their child thrive.
To help put these ideas into practice, here is a simple checklist you can adapt for your family's daily routine.
Building a Brain-Healthy Lifestyle: A Daily Checklist
This table offers a simple framework for integrating diet, exercise, and healthy habits into your child's day-to-day life. Consistency is key, so find what works for your family and stick with it.
| Habit Area | Morning Action Item | Afternoon/Evening Action Item |
|---|---|---|
| Nutrition | Start with a protein-rich breakfast (eggs, yogurt, smoothie). | Offer a brain-boosting snack (nuts, seeds, fruit). Include lean protein and colorful veggies with dinner. |
| Movement | A quick 10-minute walk or stretching session before school. | At least 30-60 minutes of active play (bike ride, park, sports). |
| Sleep Hygiene | Maintain a consistent wake-up time, even on weekends. | Start a calming wind-down routine 1 hour before bed (no screens). |
| Screen Time | Keep mornings screen-free to encourage focus for school. | Set clear limits on recreational screen time and stick to them. |
Remember, the goal isn't perfection but progress. Small, consistent daily habits can add up to make a big difference in supporting your child's overall well-being and ADHD management.
Disclaimer: This information is for educational purposes only and is not intended to diagnose or treat any medical condition. Always consult with a qualified healthcare professional when discussing medications, supplements, or creating a treatment plan for your child.
Supplements and Brain-Boosting Activities That Help
While medication and therapy are the cornerstones of a solid ADHD management plan, a truly comprehensive, holistic approach also taps into the power of targeted nutrition and brain-boosting daily activities. These strategies are all about supporting brain function from the inside out, helping improve focus, regulate mood, and build self-control.
By layering these habits into your child’s routine, you're creating a supportive environment where they can really start to flourish. Many of these ideas are simple and affordable, giving you an active role in your child's well-being and building a foundation of health that works alongside professional medical guidance.
The Power of Omega-3 Fatty Acids
You've probably heard about omega-3s, but it's worth repeating just how important they are. Fats like EPA (eicosapentaenoic acid) and DHA (docosahexaenoic acid) are essential building blocks for the brain. They're critical for maintaining healthy cell membranes and supporting the communication lines between brain cells.
For a child with ADHD, getting enough of these nutrients can make a real difference in cognitive function and focus.
The supplement aisle can feel overwhelming, so here are a few quick tips for choosing the right type of affordable, high-quality options:
- Look for EPA and DHA Ratios: Don't just look at the total fish oil content. Check the label for the specific amounts of EPA and DHA—that’s where the brain-boosting power is. Research often suggests a higher ratio of EPA to DHA can be beneficial for ADHD symptoms.
- Check for Purity: Reputable brands will test their products for heavy metals like mercury and can provide a certificate of analysis. Look for supplements that are third-party tested (e.g., by NSF International or USP) for peace of mind.
- Consider Liquid or Gummy Forms: Let's be real—pills can be a battle. For kids, affordable liquid or gummy omega-3s are often a more palatable and fuss-free alternative.
Always consult with your child’s healthcare professional before starting any new supplement, including omega-3s. They can help you determine the right dosage and ensure it is a safe and effective part of your child’s overall integrative plan.
Exercise as Brain Medicine
Physical activity is one of the most powerful—and easily accessible—tools for managing ADHD symptoms. You can think of exercise as a natural way to boost the brain’s most important neurotransmitters.
A good, brisk session of activity increases levels of dopamine and norepinephrine, which are the same brain chemicals targeted by many stimulant medications. The result? Sharper focus, a better mood, and less impulsivity.
The trick is making movement a consistent and enjoyable part of your child’s daily life. Brain-healthy activities shouldn't feel like a chore.
- A 30-minute bike ride around the neighborhood after school.
- Jumping on a trampoline or playing tag in the backyard.
- A family dance party in the living room to burn off extra steam.
These simple, fun activities get blood flowing to the brain, help organize thoughts, and can significantly improve sleep quality—another massive factor in managing ADHD symptoms.
Building Brain-Healthy Daily Habits
Beyond specific supplements and exercise, small daily habits can have a huge impact on a child's mental health and executive function. These routines create the structure and predictability that can be incredibly calming for a mind that struggles with focus and organization.
Think about weaving some of these brain-healthy activities into your family’s life:
- Mindfulness Moments: You don't need an hour. Even just five minutes of quiet breathing or a simple guided meditation for kids can help improve focus and dial down that feeling of being overwhelmed. This is an easily implemented daily habit.
- Creative Outlets: Activities like drawing, building with LEGOs, or playing an instrument give the brain a chance to hyperfocus on a positive task. It's a fantastic outlet for creative energy.
- Structured Routines: A visual schedule for morning and evening routines can be a game-changer. It helps a child know exactly what to expect, which can reduce arguments while building life skills in organization and time management.
By combining these supportive strategies with professional medical care, you create a well-rounded, integrative plan that addresses ADHD from every angle.
Disclaimer: This information is for educational purposes only and is not intended to diagnose or treat any medical condition. Please consult with a qualified healthcare professional before making any decisions about medications, supplements, or treatment plans for your child.
Navigating Your Child's ADHD Journey Into Adulthood
Figuring out the difference between ADHD and ADD is really just the first step. The real shift happens when we recognize that ADHD is a lifelong condition, and our focus moves toward setting our kids up for long-term success. The journey doesn't just stop with a diagnosis; it evolves as your child grows, and their symptoms will change right along with them. This is why early, effective support is so crucial—it gives them the skills to thrive at every stage.
That noticeable hyperactivity you see in a young child—the constant running, climbing, and squirming—often softens over time. In a teenager or young adult, that outward energy can morph into an intense feeling of internal restlessness. They might not be physically bouncing off the walls anymore, but inside they could feel mentally scattered, anxious, or just unable to settle down.
Shifting Challenges Through Key Transitions
As school and social pressures ramp up, challenges with executive functions—things like organization, managing time, and finishing tasks—tend to become much more obvious. These struggles can hit particularly hard during big transitions, like the jump from elementary to middle school or from high school to college. The unstructured nature of adulthood can make these difficulties feel even bigger if solid coping strategies aren't already in place.
This is exactly why a supportive, integrated plan is so powerful. It's not just about managing today's symptoms but about building self-awareness and resilience for all the tomorrows. An approach that blends medical support with practical lifestyle strategies provides the strongest foundation.
The goal is to empower your child with the tools to manage their unique brain wiring. With consistent support, they can learn to navigate challenges and even leverage their strengths, paving the way for academic, social, and professional success as they mature.
A Long-Term Perspective on Symptoms
It’s also important to see how different ADHD presentations play out over time. The overall prevalence of ADHD drops from childhood to adulthood, which tells us something interesting: inattentive symptoms often hang around more subtly, while hyperactive ones tend to mellow out. One major review estimates the worldwide adult ADHD rate at 3.1%, compared to 7.2% for children.
This change really highlights how inattentive symptoms—what used to be called ADD—often persist into adulthood without the more obvious hyperactivity. It also helps explain why untreated inattentive ADHD can create bigger hurdles later in life. You can learn more about these global prevalence rates and what they mean.
Understanding this long-term view helps parents see why building healthy habits early on is so important. Things like daily brain-healthy activities, consistent exercise, and a nutrient-rich diet all help a child learn to manage their ADHD effectively as they grow into capable, confident adults.
Disclaimer: This information is for educational purposes only and is not intended to diagnose or treat any medical condition. Please consult with a qualified healthcare professional before making any decisions about medications, supplements, or treatment plans for your child.
Answers to Your Top Questions
Navigating the world of ADHD can bring up a lot of questions. As a parent, you want clear, straightforward answers. Here are some of the most common concerns I hear from families, cutting through the confusion between older terms like ADD and the way we approach ADHD today.
Is ADD Still a Real Diagnosis?
Technically, no. ADD isn't a formal diagnosis anymore. The term is outdated, but the symptoms it described—that frustrating struggle with focus, organization, and seeing things through—are absolutely real.
Today, those symptoms are officially diagnosed as ADHD, Predominantly Inattentive Presentation. This shift in language is important. It validates what you're seeing in your child and aligns it with our current medical understanding, recognizing that inattention is a core piece of the ADHD puzzle, even if hyperactivity isn't obvious.
Can My Child Manage ADHD Without Medication?
A well-rounded, holistic plan is always the best path forward. For many kids, a strategy built on a brain-healthy diet, regular exercise, consistent routines, and behavioral therapy forms the foundation for success and can make a huge difference.
However, many children achieve the best results when these lifestyle supports are combined with medication. Psychotropic medications, like stimulants or non-stimulants, work on specific neural pathways to improve how the brain functions, boosting focus and taming impulsivity. This combination often unlocks a child's full potential, helping them get more out of therapy and their daily routines. Always talk with a healthcare professional to figure out the right integrative approach for your child.
When Is It Time to Get a Professional Evaluation?
You should seek a professional opinion when you notice a persistent pattern of behavior that's getting in the way of your child's ability to function and learn. One of the biggest red flags is when these struggles pop up in multiple places, like at home and at school.
It’s true that all kids can be forgetful or energetic sometimes. But with ADHD, these behaviors are more frequent and more severe than what's typical for their age. If you're worried that your child's challenges with attention, impulsivity, or hyperactivity are consistently holding them back, an evaluation is the best way to get clarity and find a path forward.
Disclaimer: This information is for educational purposes only and is not intended to diagnose or treat any medical condition. Please consult with a qualified healthcare professional before making any decisions about medications, supplements, or treatment plans for your child.
At Children Psych, we provide compassionate, evidence-based care to help your child thrive. If you're seeking a comprehensive evaluation or a personalized, integrative treatment plan, learn more about our services.